The brain is a complex organ that controls virtually every process that regulates our bodies, including thought, memory, emotion, and motor skills. Alcohol is considered a toxin and acts like poison in the brain, causing functional impairments and behavior changes, some of which can be long-lasting. Understanding how alcohol affects the brain can help you make informed decisions related to alcohol use, and empower you to build healthier habits.
How Does Alcohol Use Affect Brain Neuropsychology?
Alcohol can impair several important brain functions, leading to both short-term and long-term consequences. Here are some of the key potential effects to be aware of:
Memory
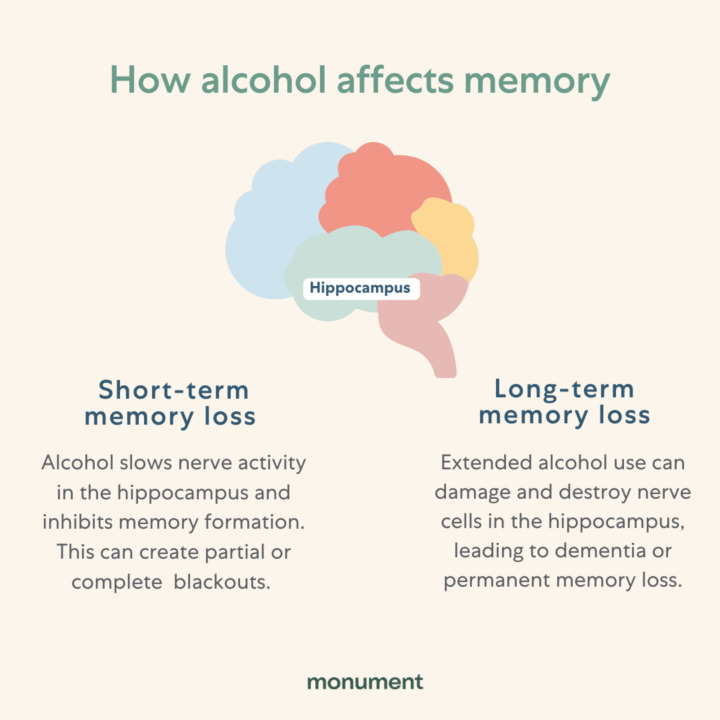
Alcohol starts to affect memory after only a few drinks. As a person’s blood alcohol content increases, so does their memory impairment. Memory is broken down into two types: short-term (i.e.: a new person’s name, items on your grocery list) and long-term (i.e.: your childhood bedroom, your wedding day.) Alcohol can make it harder to access short-term memories, and can even eradicate them entirely. This is what is commonly referred to as a “blackout.” During a blackout, the brain’s hippocampus (the area responsible for ‘storing’ memories) is impacted, and as a result, a person may only have few, if any, memories of the events surrounding drinking.
Alcohol can also have an impact on long-term memory. Over time, alcohol use can damage brain cells within the hippocampus, making it harder, or even impossible, to recollect long-term memories. This is known as alcohol-related dementia. Reducing or eliminating your alcohol consumption can help prevent memory loss and blackouts, and even repair and improve your memory.
Executive Functions
Executive function is known as the “management system” of the brain. It’s the set of mental skills that include working memory, flexible thinking, and self-control. Executive functions are generated in the prefrontal cortex of the brain. When you drink alcohol, it suppresses activity in the prefrontal cortex, causing impairments to judgment, problem solving, decision making, attention span, perception, and language. The more alcohol you drink in a sitting, the more pronounced these impairments are.
Over time, excessive alcohol use can damage brain cells within the prefrontal cortex, resulting in more long-term symptoms such as problems with processing new information, gaining new skills, and formulating plans.
Visuospatial Abilities
The occipital lobe of the brain is responsible for visuospatial processing, which is how we understand what we see around us. Everyday examples of visuospatial tasks include driving a car and walking up and down stairs. Because alcohol is a depressant, it slows down and impairs your visuospatial abilities. This is why someone who is intoxicated may have difficulties locating objects, reading, and recognizing depth perception (i.e.: they may be bumping into things).
Over time, alcohol use can lead to long-term impairments, such as a decrease in peripheral vision (impacting depth perception) and in very rare cases, vision loss. While this symptom is well-documented, more research is needed to understand exactly why this occurs.
Mental Health
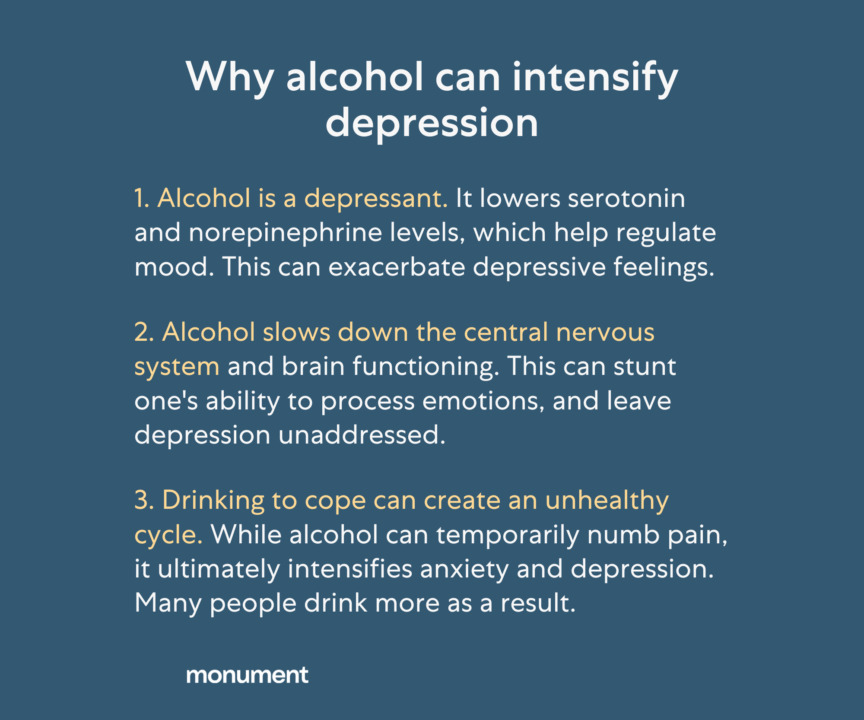
Alcohol can affect your mental health in a variety of ways. It impacts the striatum, the area of the brain that produces feelings of reward and pleasure, and also the amygdala, the area of the brain responsible for emotions. This can create an unhealthy cycle of relying on alcohol to experience a sense of joy or elation. While alcohol can provide relief in the short term, it ultimately leads to increased discomfort. Alcohol use disrupts and depletes hormones that impact our mood, which can lead to a spike of anxiety when we stop drinking (also known as ‘hangxiety’). Lastly, as seen in the graphic below, it can exacerbate feelings of depression in both the short and long term.
Psychomotor Abilities
‘Psychomotor’ refers to the connection between your brain and your muscles. Alcohol’s impact on both the parietal lobe and the cerebellum of the brain creates a disconnect between the brain and body, and results in impaired coordination, slowed reaction times, difficulties with balance, and poor hand-eye coordination.
Over time, unhealthy alcohol use can create more permanent impairments to these brain areas, resulting in psychomotor consequences even when someone is not intoxicated. These effects can include a slower reaction time for hand-eye coordinated tasks, and also an instability in gait, putting a person at greater risk for falls and injury.
Does Alcohol Actually Kill Brain Cells?
Experts argue that drinking does not actually lead to brain cell, or neuron, death – but does lead to a breakdown in cell communication. Alcohol makes it harder for brain cells to fire electrical messages, which are essential for normal brain communication and function. This causes acute impairments like slurred speech and slowed reaction time.
Over time, alcohol use can cause more lasting damage to dendrites, the part of the neuron that receives electrical messages, which results in a more permanent breakdown in communication between neurons. Despite this, research has shown that prolonged abstinence from alcohol can help recover neuron function, and therefore improve functional abilities.
While alcohol doesn’t actually ‘kill’ brain cells, it can prevent your brain cells from properly communicating. It can also prevent the formation of new brain cells and can shrink your brain tissue. Let’s dive deeper into those last two:
Neurogenesis Interference
Research has shown that specific areas of the brain are able to continue to form new cells throughout your entire life. This process is called ‘neurogenesis.’ Although alcohol does not actually ‘kill’ brain cells, high levels of alcohol can prevent this formation of new brain cells. During periods of abstinence, neurogenesis is able to resume again, allowing for increased functionality within the brain.
Brain Shrinkage
Long term alcohol use is often associated with brain shrinkage, or atrophy. More specifically, grey matter (one of two types of tissue within the brain) has been noted to be both smaller and lighter in the brains of those who have a history of long-term alcohol use. Remarkably, research also supports that long-term sobriety can either partially or fully reverse this shrinkage. One study even showed that improvement to the volume of grey matter can occur in as little as three weeks of sobriety.
Can You Recover From Alcohol-Related Brain Damage?
The brain has an incredible capacity to heal itself. The key is to give it time away from the toxin of alcohol in order to restore neuron communication, grey matter, and other key areas of functioning. Research shows that the brain can start recovering after three weeks without alcohol, and return to a healthy state after one year of sobriety. Of course, everyone’s alcohol recovery timeline is different. In some cases, damage can’t be reversed. This is especially true for those who drank heavily for a significant period of time. It’s never too early to seek support and take preventative steps so that permanent damage can be avoided.
Use of Neuroscience in Alcohol Treatment
Alcohol use disorder is a medical condition influenced by biological, psychological, and social factors. There are several treatment methods that have been informed by neuroscience and proven to be effective options. Let’s take a closer look at a few:
Medication to Stop Drinking
There are multiple medications approved by the FDA to help an individual stop drinking. One of the most effective and widely studied medications is naltrexone. When you have a drink, your brain releases dopamine, the ‘feel-good’ hormone. This causes the brain to associate alcohol with pleasure, and to crave more of it. Naltrexone works by indirectly blocking the release of dopamine so that you don’t get the same euphoric feelings from drinking. Over time, the strong associations in the brain between alcohol and pleasure begin to weaken, causing fewer alcohol cravings. This can help someone start to drink less and have more brain space to focus on other aspects of recovery.
Cognitive Behavioral Therapy
Therapy can be another helpful tool for helping to change your relationship with alcohol. Cognitive Behavioral Therapy (or ‘CBT’) is proven to help reduce heavy drinking days and overall alcohol consumption.10 CBT can also help an individual navigate many other aspects of recovery, including:
- Learning healthy coping skills for managing triggers and cravings for alcohol
- Restructuring unhelpful thought patterns
- Addressing co-occurring anxiety and depression
As explained above, alcohol use disorder can temporarily affect your motivation and decision making processes. Because of this, it can be difficult to achieve and maintain sobriety using willpower alone. Getting support from a mental health professional can help you work through each unique challenge faced with expert guidance.
Gaining a better understanding of how alcohol impacts the brain can be overwhelming, but can also be an eye-opening experience. Knowledge is powerful, and it is important to remember that you don’t have to navigate this journey alone. At Monument, you can work with licensed therapists and physicians trained in helping people change their drinking habits. You can also connect with a community of others who share similar experiences. We’re here for you!
Sources:
- American Addiction Centers. “Wet Brain from Alcohol: Signs & Symptoms of Wernicke-Korsakoff Syndrome, https://americanaddictioncenters.org/alcoholism-treatment/wet-brain.” Accessed September 2, 2022.
- Ind J Priv Psychiatry. “Impairment of Executive Function in Alcohol Dependent Persons, https://www.ijiapp.com/doi/IJPP/pdf/10.5005/jp-journals-10067-0010.” Accessed September 2, 2022.
- J Stud Alcohol. “An effect of alcohol on the distribution of spatial attention, https://pubmed.ncbi.nlm.nih.gov/8709584/.” Accessed September 2, 2022.
- The Lancet. “Do alcoholics drink their neurons away?, https://www.thelancet.com/journals/lancet/article/PII0140-6736(93)92185-V/fulltext.” Accessed September 2, 2022.
- Journal of Studies on Alcohol. “Visuospatial perception, construction and memory in alcoholism, https://pubmed.ncbi.nlm.nih.gov/8683962/.” Accessed September 2, 2022.
- Scientific American. “What are the effects of alcohol on the brain?, https://www.scientificamerican.com/article/what-are-the-effects-of-a/.” Accessed September 2, 2022.
- Drug Alcohol Depend. “Effects of alcohol on psychomotor performance and perceived impairment in heavy binge social drinkers, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2764986/.” Accessed September 2, 2022.
- The American Journal of Psychiatry. “Neuroscience of Addiction: Relevance to Prevention and Treatment.” https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2018.17101174. Accessed September 2, 2022.
- ScienceDirect. “Neuropsychological deficits in alcohol use disorder, https://www.sciencedirect.com/science/article/pii/B9780128152980000083.” Accessed September 2, 2022.
- Addiction. “Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: a meta-analysis, https://pubmed.ncbi.nlm.nih.gov/24304463/.” Accessed September 2, 2022.
Naltrexone has the capacity to cause hepatocellular injury (liver injury) when given in excessive doses. Naltrexone is contraindicated in acute hepatitis or liver failure, and its use in patients with active liver disease must be carefully considered in light of its hepatotoxic effects. In the treatment of alcohol dependence, adverse reactions include difficulty sleeping, anxiety, nervousness, abdominal pain/cramps, nausea and/or vomiting, low energy, joint and muscle pain, headache, dizziness and somnolence. This is not a complete list of potential adverse events associated with naltrexone hydrochloride. Please see Full Prescribing Information for a complete list.
