Alcohol shakes, also referred to as hangover shakes or tremors, are a potential symptom of alcohol withdrawal. When your body gets used to drinking excessively, it can become reliant on alcohol to maintain its balance. Because of this alcohol dependence, suddenly reducing your consumption (whether quitting alcohol cold turkey or practicing moderation), can result in a variety of alcohol withdrawal symptoms including trembling that typically affects the hands. Alcohol shakes can be a sign of mild or severe alcohol withdrawal, most frequently occurring 6-24 hours after alcohol was last consumed before reaching their peak within 24 to 72 hours.¹
Seeking more information about alcohol shakes or tremors is helpful in understanding physical alcohol dependence and identifying safe steps for cutting back on drinking. However, if you believe you are currently experiencing shakes, tremors, or any other alcohol withdrawal syndrome side effects, please contact your health care provider immediately. If this is a medical emergency, please call 911.
For those looking for non-urgent information about shakes and tremors to inform conversations with your healthcare provider and/or loved ones, continue reading to learn more about the causes and signs of these alcohol-induced symptoms. To understand why alcohol shakes occur, let’s dive into the brain chemistry of withdrawal.
The Chemical Explanation Behind Alcohol Withdrawal
Alcohol can affect brain chemistry while we are drinking and after we stop. Frequently asked questions from my patients include ‘is alcohol a stimulant or depressant?’ and ‘why do I feel so horrible when I stop drinking?’ A sudden cessation or reduction in alcohol intake can lead to alcohol shakes and tremors, among other alcohol withdrawal symptoms. That’s why before you cut back on consuming alcohol, it’s crucial that you connect with a health care provider to discuss your safest course of action. Regardless of your drinking habits, whether you classify them as long-term daily use, binge drinking, or otherwise, it’s always recommended to check in with a professional. Now, let’s dive into the chemistry of alcohol withdrawal.
In a normal state, your brain keeps you alert and calm by keeping what’s called your inhibitory and excitatory systems in balance. This is also known as E-I balance. Alcohol throws off this balance by enhancing the activity of a major inhibitory chemical in your brain called GABA, resulting in you feeling relaxed and drowsy. As you continue to drink regularly and spend more time in the inhibited state, your brain tries to find E-I balance again. The brain seeks this balance by reducing your natural inhibitory activity (because alcohol is already unnaturally increasing inhibitory chemicals) and increasing excitatory activity.
When you suddenly stop drinking or decrease alcohol consumption significantly, you remove the unnatural inhibitory chemicals, and your inhibitory and excitatory systems are imbalanced. Your inhibitory system is depressed, and your excitatory system is overly enhanced. This leads to an overexcitation of your brain and the development of signs and symptoms of alcohol withdrawal, including the possibility of shakes, tremors, and other symptoms.

Symptoms of Alcohol Withdrawal
Alcohol withdrawal can have mild to severe symptoms. Severe withdrawal symptoms can be life-threatening, and it’s crucial to both be aware of them, and discuss potential risks with your healthcare provider.
Alcohol shakes and tremors
One possible symptom is alcohol shakes and tremors, which refers to an uncontrollable shaking or involuntary quivering, commonly in the hands and feet. In addition to alcohol withdrawal shakes and tremors, people may experience anxiety, sweating, agitation, headache, nausea, and vomiting.
About 80% of people who are dependent on alcohol experience withdrawal symptoms to some degree, though most improve within a week without complications.² However, in more severe cases, people may have auditory, visual, or tactile hallucinations, among other symptoms. A common tactile hallucination is feeling a bug crawling under your skin. If you’re experiencing symptoms, including shaking hands when not drinking alcohol, you should check in with your healthcare provider. They will work with you to provide the safest course of action, and also provide relief by answering your questions.
Practicing self-compassion while changing your relationship with alcohol
Hallucinations
Hallucinations can occur without any prior symptoms and are most likely to develop 8 hours after the last drink and peak at 24-96 hours.² If you believe you are experiencing withdrawal symptoms, you should seek medical attention immediately at your local emergency room and call 911 in case of emergency.
Seizures
In addition to hallucinations, seizures are another potentially severe symptom of alcohol withdrawal. Withdrawal-related seizures can occur even if you don’t have other symptoms. Seizures can begin as early as 12 hours after the last drink and can last up to 48 hours.² About 5-15% of people withdrawing from alcohol develop seizures.²
The risk is the greatest for people who previously had seizures and those withdrawing from other sedatives such as benzodiazepines. When navigating alcohol treatment, it’s especially important to accurately share your medical history and alcohol consumption history with your provider, so that they can provide the safest and most appropriate care for you. Hallucinations and seizures can also be part of a severe alcohol withdrawal response known as delirium tremens.
What is the Difference Between Delirium Tremens (DTs) and Tremors?
Delirium tremens (DTs) is among the most severe and potentially life-threatening symptoms of alcohol withdrawal. As the name suggests, the signs of delirium tremens include confusion, disorientation, fever, high blood pressure, rapid heartbeat, and drenching sweats. Withdrawal delirium typically begins between 1 to 3 days after the last drink and peaks on the 4 to 5th day.²
As a physician on the Monument platform, I often hear patients confuse DTs with tremors when first learning about alcohol withdrawal. While DTs symptoms may include alcohol tremors and shakes, DTs is also characterized by other signs of severe alcohol withdrawal, like high blood-pressure and seizures. In comparison, alcohol tremors and shakes are more common than DTs, and can be a sign of mild or severe withdrawal.

Are Withdrawal Symptoms a Sign of Alcohol Use Disorder or Alcohol Dependence?
Another question I’m often asked by my patients is ‘are withdrawal symptoms a sign of alcohol use disorder or alcohol dependence?’ Many people use the terms alcohol dependence and alcohol use disorder interchangeably, but they are not the same.
Alcohol dependence and withdrawals
Technically, alcohol dependence refers to having withdrawal symptoms due to the cessation or reduction of alcohol consumption. So, in brief, alcohol withdrawal symptoms are a sign of alcohol dependence. However, if you experience withdrawal symptoms, you may also meet the clinical criteria for alcohol use disorder, or ‘AUD.’
Alcohol use disorder and withdrawals
Defined by National Institute on Alcohol Abuse and Alcoholism (NIAAA) as “a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences,” experiencing withdrawals is one of the criteria used to diagnose alcohol use disorder. An individual needs to meet two of eleven criteria outlined by the American Psychiatric Association to be diagnosed with AUD, which may or may not include withdrawal symptoms.
However, having withdrawals is a strong indication that you’ve been drinking heavily for a prolonged period, and that there is a higher chance of developing or having AUD. To take an AUD assessment, you can sign up for the Monument Community. If you do meet the criteria for alcohol use disorder, it’s essential to understand that treating alcohol withdrawals is not a treatment for alcohol use disorder. It’s undoubtedly a critical first step in your recovery, but you will likely want to engage in longer-term treatment and support to treat alcohol use disorder itself.

How to Treat Alcohol Shakes and Other Withdrawal Symptoms
The safest way to prevent dangerous withdrawal symptoms is to consult with a medical professional to assess your risk and align on the appropriate level of care. Depending on the risk level, medical withdrawal management, commonly known as “detox ,” may be recommended. Supervised alcohol detox may require medication and frequent monitoring to be done safely. Furthermore, other medical conditions can mimic acute alcohol withdrawal or post-acute alcohol withdrawal, so it’s important to get immediate medical attention to receive accurate diagnoses and care.
It’s difficult to predict the course of acute alcohol withdrawal symptoms, which is why it’s recommended to seek expert guidance. Some people have very mild symptoms that resolve quickly, while others have more severe and prolonged courses. There is also the possibility that an individual develops prolonged withdrawal symptoms, also known as post-acute withdrawal syndrome (PAWS), which can last a few weeks to a few months. You can learn more about withdrawal, and PAWS specifically, by taking a closer look at the alcohol recovery timeline.
Long-term Online Alcohol Treatment
Seeking support to change your relationship with alcohol is something to be proud of, and working with a physician and therapist is a great way to prioritize your health and safety. If in-person supervised alcohol detox is recommended due to the risk of alcohol withdrawal, you are not alone. After safely completing detox and reducing the risk of alcohol withdrawal, many people pursue longer-term care such as online alcohol treatment. Monument connects you to physicians like myself, and licensed therapists who can help you build a treatment toolkit to empower your long-term success.
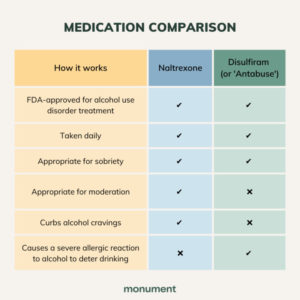
That treatment toolkit may include medication to stop drinking, online alcohol therapy, and/or alcohol support groups. In addition to working with an expert Care Team, finding community with other people with shared challenges and experiences can provide additional encouragement and accountability. Regardless of your pathway to recovery, your experience is valid, and you deserve to feel safe and supported. To connect with a physician to discuss your personal needs and goals, explore your treatment plan options today.
Sources:
- National Library of Medicine. “Novel Algorithms for the Prophylaxis and Management of Alcohol Withdrawal Syndromes-Beyond Benzodiazepines, https://pubmed.ncbi.nlm.nih.gov/28601135/.” Accessed Aug. 25, 2021.
- Res World. “Kindling in
Alcohol Withdrawal, https://pubs.niaaa.nih.gov/publications/arh22-1/25-34.pdf.” Accessed Aug. 25, 2021.